“They Seem Fine…” – The Danger of Invisible Wounds
“Trauma in children rarely looks like adults expect. While some cry or act out, others become ‘perfectly quiet’ or ‘helpful beyond their years.’ These adaptations are survival strategies – not resilience.”
— Dr. Naomi Chen, WellChild Haven Trauma Specialist
A Startling Reality:
- 1 in 4 children experience trauma before age 4 (National Child Traumatic Stress Network)
- Only 20% show obvious symptoms like aggression or nightmares (Journal of Pediatric Psychology, 2024)
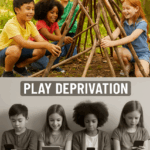
8 Silent Signs of Unprocessed Trauma
(Often mistaken for “phases” or behavioral issues)
- Hyper-Compliance
Excessive eagerness to please, fear of making mistakes
Red Flag: “Sorry!” muttered constantly over minor incidents - Developmental Regression
Bedwetting, baby talk, or clinginess in previously independent kids - Somatic Mysteries
Unexplained stomachaches/headaches with no medical cause - Play Repetitions
Re-enacting distressing themes (e.g., dolls “getting hurt”) without emotional release - Frozen Watchfulness
Scanning rooms intensely, flinching at sudden movements - Dissociative Habits
“Zoning out” for long periods, losing time, imaginary friends at older ages - Food Rituals
Hoarding snacks, obsessive chewing, or aversion to certain textures - Pseudomaturity
Over-caring for siblings/pets while neglecting own needs
Key Insight: Trauma lives in the body. These signs indicate a nervous system stuck in “survival mode.”
Age-Specific Manifestations
| Age | Common Trauma Response | Often Misdiagnosed As |
|---|---|---|
| Toddlers | Hair-pulling, head-banging | Autism spectrum |
| 5-9 yrs | “Accident-prone” behavior | ADHD |
| Tweens | Perfectionism, excessive guilt | Anxiety disorders |
| Teens | Self-harm, risky sexual behavior | Depression/BPD |
Why Missed?
Educators and doctors rarely ask:
- “Has your child witnessed violence?”
- “Did they experience a sudden loss or medical trauma?”
Your Response Toolkit: 4 Trauma-Informed Steps
???? 1. Safety First
Script: “You’re safe now. My job is to protect you.”
(Avoid: “Why didn’t you tell me sooner?”)
???? 2. Body Awareness
Activity: “Point to where the worry lives in your body” (using a gingerbread man outline)
???? 3. Predictable Rhythms
Implement: Visible daily schedules + 10-minute “connection windows” (no screens)
???? 4. Co-Regulation
Technique: Bubble Breathing
“Smell the flowers (inhale), blow bubbles (exhale)” – do it WITH them
When to Seek Professional Help
WellChild Haven’s Child Trauma Team specializes in:
- Forensic Interviews: Uncover abuse without retraumatizing
- Somatic Therapy: Release trauma through play/sensory activities
- Family Systems Repair: Break cycles of generational trauma
Our Evidence-Based Approach:
Diagram
Code
Download
Safety & Trust Building
Body-Based Regulation
Trauma Narrative Processing
Integration & Post-Traumatic Growth
“After our foster son’s food hoarding was revealed as trauma-driven, WellChild Haven’s OT taught him ‘safety signals’ at mealtimes. He now eats without panic.”
— The Davies Family
Take Action Today
Free Resource:
????️ [Download: “Trauma Response Cheat Sheet: What to Say/Do in Crisis Moments”]
Confidential Assessment:
???? [Book a Trauma Screening Consultation]
$160 | Sliding scale available
24/7 Crisis Support:
☎️ Call our Child Protection Hotline: (555) 123-SAFE
(Immediate intervention for abuse disclosures)
Faith Integration
“He heals the brokenhearted and binds up their wounds (Psalm 147:3). At WellChild Haven, we believe sacred spaces of safety allow God’s healing to begin – mind, body, and spirit.”
— Chaplain Sarah Williams
Footer Note:
WellChild Haven’s trauma team includes forensic pediatricians, licensed therapists, and trauma-informed clergy. All services comply with state mandatory reporting laws.
Categories: Child Protection, Trauma Recovery, Mental Health
Tags: hidden trauma signs, childhood PTSD symptoms, trauma therapy for kids, somatic healing